Is Your Provider Registry Your Most Strategic Asset, or Your Biggest Bottleneck?
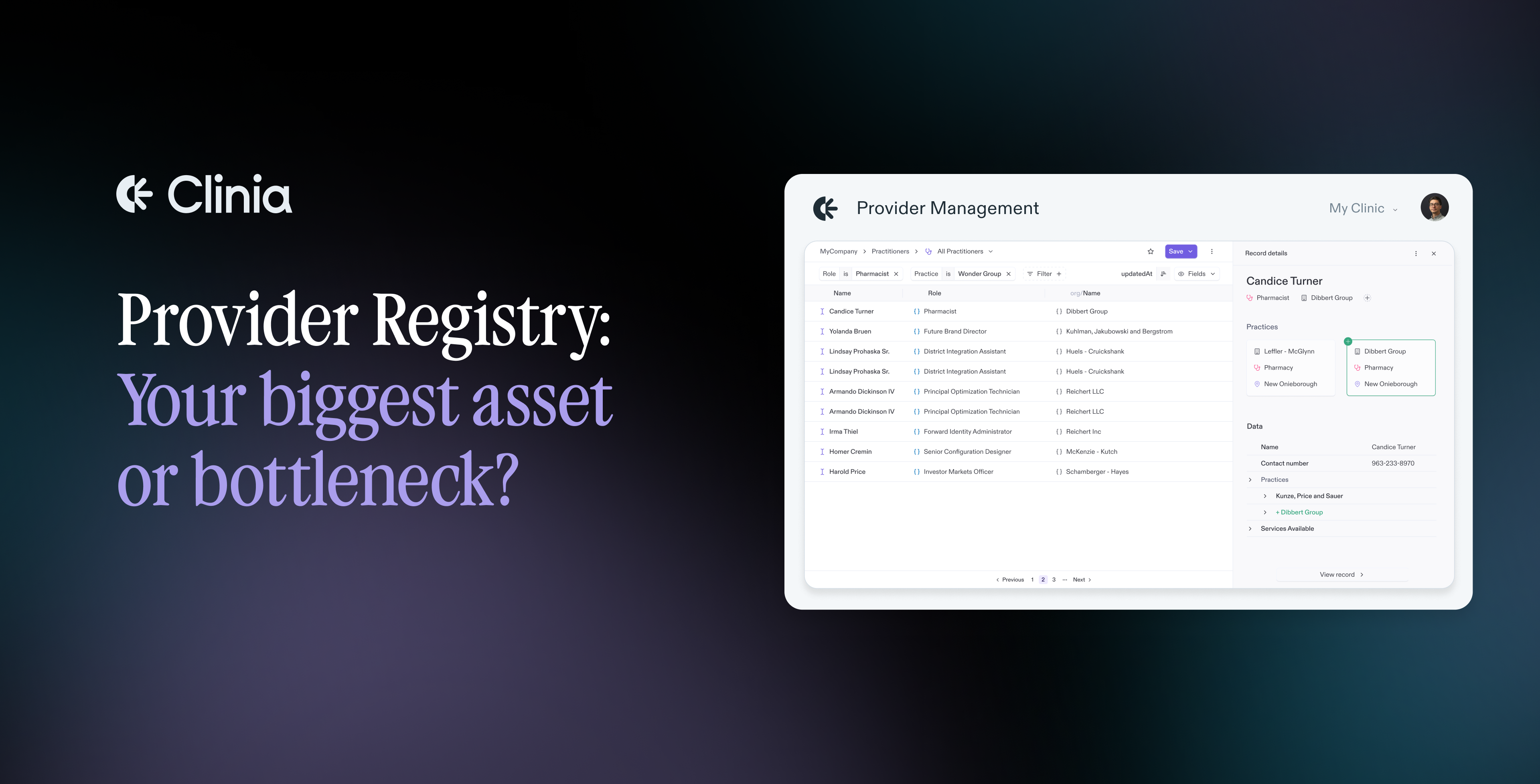
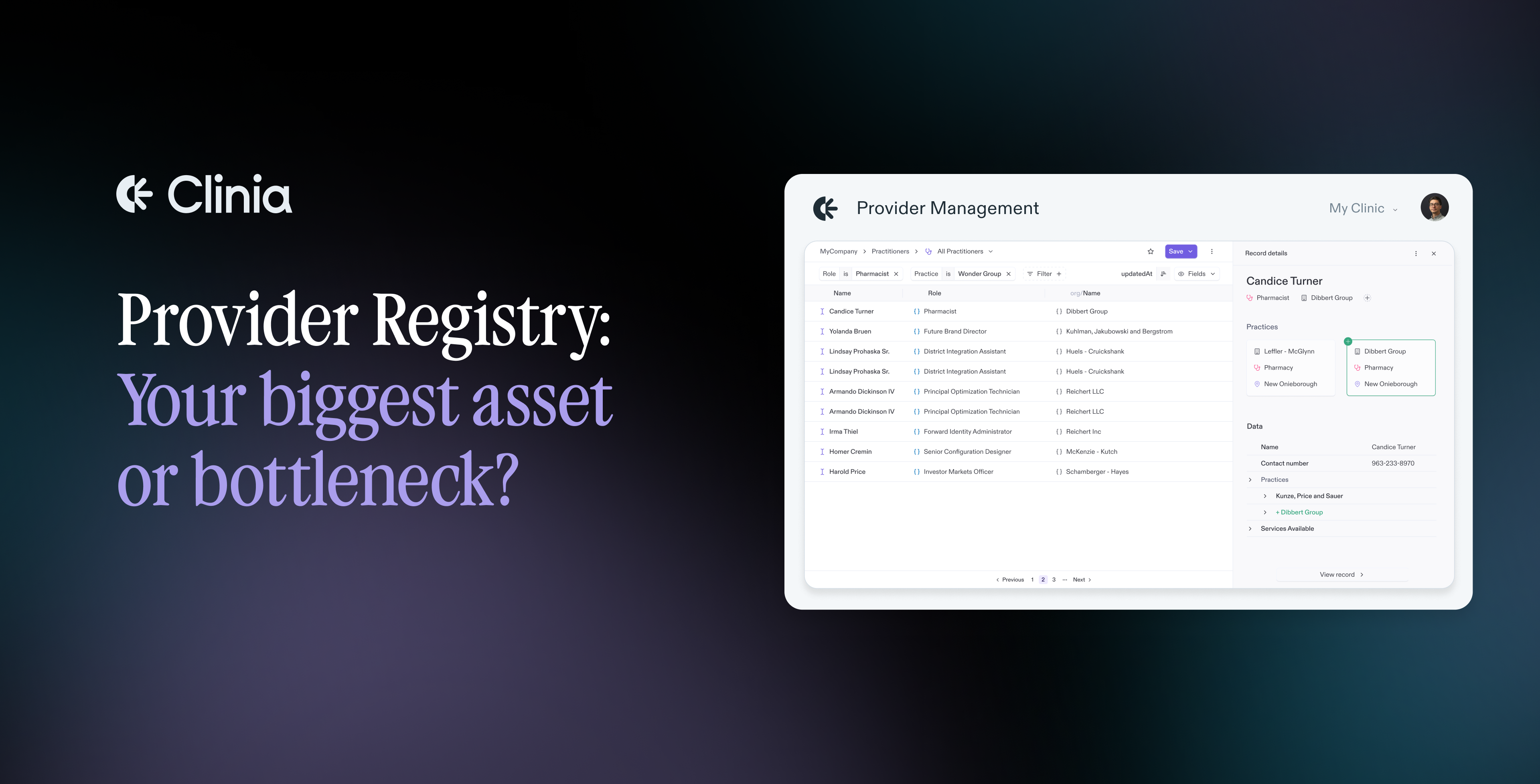
Provider registry is an essential component of the health system as it powers nearly every interaction in healthcare. From search and scheduling to referrals, claims, and care coordination, it’s the foundation that systems and people rely on to make decisions and deliver services. Still, many organizations are finding that maintaining accurate, connected provider data is harder than ever.
In this article, we break it down into three parts: what’s changing in provider data, why the old approach no longer works, and what organizations need to do to stay ahead.
AI-enabled healthcare runs on real-time data. Healthcare now generates massive volumes of real‑time data, powered by artificial intelligence, streaming workflows and digital care delivery [4]. As AI tools like voice assistants and predictive triage reshape care delivery, provider data can no longer be static. These systems rely on real-time information—availability, specialties, services—to function safely and effectively.
Modern users expect more from search interfaces. Expectations around provider search have evolved—patients, members, and referring clinicians now demand fast, intuitive, and information-rich directories. Yet, a 2023 US study revealed a persistent gap between what users need and what directories provide. Only 58% listed office hours and 59% noted disability access; 7% didn’t specify whether providers were accepting new patients, despite federal requirements [5]. In parallel, the scope of required provider data is expanding—users increasingly rely on directories that include specialties, sub-focus areas, telehealth availability, languages spoken, and care modalities to support informed decision-making.
More data, more sources, more scale. Today’s providers operate across multiple care networks, delivery modes (like in-person, virtual, or home care), and digital platforms, which results in a massive flow of inconsistent data from many sources. Managing this scale with static files and siloed systems leads to duplication, delays, and errors. Without flexible infrastructure, provider data becomes a liability, not an asset.
As healthcare systems evolve, they rely more than ever on contextual, interconnected data. Without trustworthy provider information embedded within core workflows, ambitions like intelligent referrals and real-time navigation remain difficult to operationalize.
Manual updates are still the norm and they block progress. While some level of manual work will always be necessary, relying too heavily on it remains a major obstacle in maintaining accurate provider directories. A recent study showed that the administrative burden for physician practices—submitting data through different technologies, schedules, and formats—costs practices and insurers nearly US $2.76 billion annually [6]. The fragmented update requirements place ongoing strain on resources and undermine the reliability of directory data.
Flat‑file ingestion and rigid static schemas were built for a slower, static era of data management. They rely on batch updates and fixed structures that can’t keep up with the real-time, multi-source demands of modern provider networks. As data changes frequently and comes in many formats, these outdated models create delays, inconsistencies, and high maintenance costs, making it harder to deliver accurate, workflow-ready information when it’s needed most.
Too many sources, too many truths. The average provider registry isn’t a single source of truth—it’s often a patchwork of directories, spreadsheets, lists, and siloed systems. Inaccurate contact details and outdated entries, including so-called “ghost” providers who are no longer practicing or accepting patients, remain widespread issues. Listed practice locations often contain inaccuracies in address, phone number, or specialty information. A 2024 study published in Health Affairs Scholar showed that contact information across major insurer directories was inconsistent in about 35–53% of cases, and indicated that inaccuracies are not only common but persistent over time [1].
The multi‑format update burden for provider registries is real and significant. When credentialing feeds, payer data, internal HR systems, and legacy directories each use different formats, standards, and timelines, what appears consistent in one system may conflict in another. In fact, a large study found that across five major US insurer directories, consistency of address information varied from only 16.5 % to 27.9 %, and phone‑number consistency from 16.0 % to 27.4 %—clear evidence that format and standard fragmentation remains a systemic problem [2]. This format variation slows teams, adds manual overhead, and escalates technical debt across the provider data lifecycle.
Even clean data can fail to deliver value if it isn’t actionable. Many organizations invest in correcting provider records for accuracy—standardizing names, updating contact details, removing duplicates—but this “tidied” data often remains disconnected from the workflows it’s supposed to support. When provider data is not standardized, interoperable, or linked to downstream systems, it cannot effectively power intelligent features such as personalized navigation or AI-based recommendations, even when it is accurate. Without open APIs, common standards such as FHIR, and real-time access, this data remains siloed and loses much of its operational value. As recent research confirms, meaningful clinical data exchange lags behind technical advances [3].
Compliance with federal mandates like the No Surprises Act adds further pressure. Failure to meet these standards subjects organizations to severe regulatory penalties, costly administrative appeals, and mounting claim denials. This elevates the challenge from a simple technical burden to an executive-level risk management issue.
The cracks in the old models aren’t just signs of decay—they’re signals for transformation. As healthcare systems move toward greater interoperability, patient-centricity, and data transparency, provider data management must evolve to match this new reality.
Solving provider data challenges starts with rethinking the role of provider data. Rather than treating it as an administrative record to be cleaned and stored, leading health organizations are beginning to see provider data as live infrastructure: a dynamic asset that can adapt, respond, and power critical workflows across the ecosystem.
To support this shift, provider registries must be reimagined around three core principles: how data is connected, how it’s managed, and how it’s activated.
Connect: break silos without forcing standardization. The average provider registry pulls from credentialing feeds, payer files, internal HR systems, and legacy directories—each with its own schema and update cycle. A modern registry must integrate data from diverse sources without requiring standardization upfront, instead using flexible schemas and mapping logic that can ingest data continuously and reconcile it into a single, up-to-date source of truth.
This architecture enables data to flow without friction even when scale and variety increase.
Manage: clean, traceable records with smart automation. Cleaning data doesn’t have to mean reviewing everything manually. With configurable rules, deduplication logic, and smart automation powered in part by AI, most entries can be processed automatically, with only exceptions flagged for leveraging Human-in-the-Loop technology. This dramatically reduces operational overhead and allows experts to focus where their judgment adds the most value.
At the same time, a modern system must preserve traceability, maintaining links back to original source data so teams can see where information came from, compare versions, and trust the logic behind what they’re using.
Activate: deliver the right data to the right workflow, in real time. Clean data is only valuable if it can be used. Modern provider data platforms must allow flexible partitioning based on geography, business logic, access levels, or compliance rules, and must support secure, real-time APIs that feed information directly into search, referrals, directories, analytics, claims, or care navigation systems.
This is the layer where provider data stops being passive and becomes active infrastructure, enabling personalized experiences, coordinated care, and intelligent automation.
Interoperability, scale, and intelligence demand more than a tidy directory. They require a new mindset—one where provider data is seen not as a liability to manage, but as a strategic capability to deliver results at scale.
Clinia contributes to this shift with a provider data platform built for integration, automation, and scale. Regardless of the tools used, the path forward is clear: organizations that approach provider data as infrastructure—not just information—will be better positioned to support evolving care models and technologies.
[1] Haeder SF, Zhu JM. Inaccuracies in provider directories persist for long periods of time. Health Aff Scholar. 2024;2(6).
[2] Butala NM, Jiwani K, Bucholz EM. Characterizing physician directory data quality: variation by specialty, state, and insurer. BMC Health Serv Res*.* 2024;24:808.
[3] Pimenta N, Chaves A, Sousa R, Abelha A, Peixoto H. Interoperability of clinical data through FHIR: a review. Procedia Comput Sci. 2023;220:856-861.
[4] Shaffi SM. Transforming healthcare with real-time big data analytics: opportunities, challenges, and future directions. Int J Fundam Manag Res. 2025;7(1).
[5] Xu WY, Raver EW, Elton T IV, Davis M, Haeder SF. Disconnects between provider network directories and patient preferences. Am J Manag Care. 2024;30(12):660–666.
[6] Butala NM, Jiwani K, Bucholz EM. Consistency of physician data across health insurer directories. JAMA Netw Open. 2023;6(4):e2802329.